Anatomy of Common Peroneal Nerve
Common peroneal nerve comes off the sciatic nerve in the thigh. It then courses around the fibular neck and bifurcates into:
- Deep peroneal nerve
- Innervates the anterior compartment of the leg » dorsiflexes ankle and extends toes
- Provides sensation to the first dorsal webspace
- Superficial peroneal nerve
- Innervates the lateral (peroneal) compartment of the leg » everts foot and plantarflexes ankle
- Provides sensation to anterolateral distal third of the leg and the majority of dorsum of the foot (except the first webspace)
Common peroneal nerve palsy may be due to:
- Traumatic causes
- Knee dislocation
- Direct impact or cut on the fibular neck
- Following surgery to the knee
- Atraumatic causes
- Entrapment neuropathy
- Intraneural ganglion
- Peripheral nerve tumour
- Systemic illnesses (diabetes mellitus, inflammatory conditions, motor neuron disease)
Foot Drop
Foot drop may occur if there is dysfunction of the nerve supply controlling dorsiflexion of ankle. The common sites of involvement are either at the spine (lumbar nerve roots) or at the knee (common peroneal nerve). Specifically, when the peroneal nerve is involved, it is the deep branch that is responsible for the loss of action.
Consequences of foot drop
- the affected foot catches on the floor when walking
- high stepping gait - the affected leg is lifted high to clear the floor
- swinging of the affected leg to clear the floor
Key message
Common peroneal nerve palsy is only one of the many possible causes of foot drop.
Presentation
- Foot drop often is the most striking feature
- Weakness in foot eversion may occur if the superficial peroneal component is involved
- The pattern of sensory loss would suggest either superficial or deep peroneal nerves or both are involved
- Tinel's sign is a reliable clinical sign to localise area of nerve irritation or entrapment - Tapping along the course of the nerve (particularly around the fibular neck) causing shooting pain and tingling into the foot
Investigations
- Neurophysiology is used to confirm the diagnosis
- Radiographs of the knee
- MRI to look for lesions compressing the nerve
Treatment
Nonoperative
- Ankle-foot orthoses
- Physiotherapy
Operative
- In atraumatic situations, if there is strong indication of a focal nerve lesion (positive Tinel's spot that is not advancing with time), exploration and neurolysis are recommended.
- In open injury, the nerve needs to be explored and repaired if necessary.
- In closed injury, judgement is required regarding the potential severity of the nerve lesion in order to decideupon the period of observation (waiting for spontaneous recovery). If in doubt, exploration is recommended.
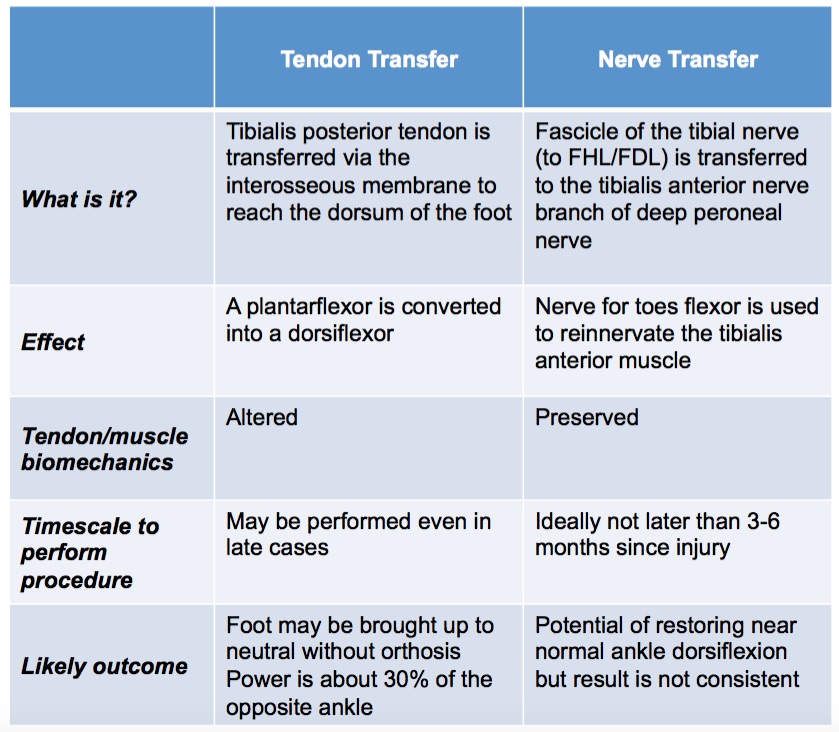
- Following knee dislocations, a long segment of the nerve may have been stretched/injured. Reported outcomes of neurolysis or nerve grafting have been poor. This is probably related to the length of nerve graft and the level of energy involved in the initial injury. Other reconstructive options include tendon transfer or nerve transfer.
Management of common peroneal nerve injury associated with traumatic knee dislocation.pdf