Anatomy of Posterior Interosseous Nerve (PIN)
- ECRB is innervated by the radial nerve in 50% of cases and by the PIN in 50% of cases.
Aetiology of PIN Palsy
There are two major groups of patients:
- Traumatic
- Fractures around the elbow
- Lacerations with direct nerve injuries
- Direct contusions from blunt trauma
- Atraumatic
- Entrapment neuropathy
- Neuralgic amyotrophy (Parsonage-Turner Syndrome)
- Hourglass constrictions of the PIN
- Space-occupying lesions (lipoma, ganglion, inflammatory arthropathy)
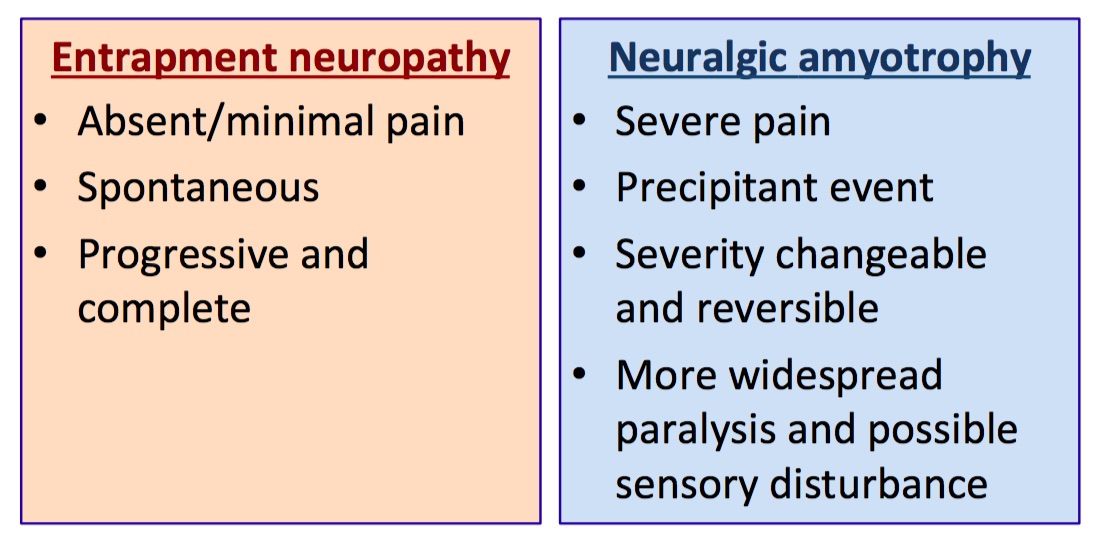
Among the atraumatic cases, there are certain clinical features that might point towards a particular aetiology:
Presentation
In traumatic situations, the combination of elbow trauma with the following signs should alert the clinician to the possibility of injuries to the PIN:
- weak wrist extension with radial deviation
- extension loss at the metacarpophalangeal joints of all the fingers and thumb
- weak abduction of the thumb
In atraumatic cases, patients may present with
- Aching pain over the proximal dorsoradial forearm
- Tenderness over the radial tunnel
- Motor weakness/paralysis as outlined above
- The presentation may be variable or progressive
Investigations
- Radiographs - necessary in elbow trauma but less useful in atraumatic cases
- MRI - utilised to exclude any space-occupying lesions, may show denervated changes in the muscles
- Neurophysiology - performed after 2-3 weeks of onset of palsy
Treatment
-
In traumatic cases,
- if there is an open wound over the course of the PIN with dysfunction, formal exploration and repair of the nerve are indicated.
- in elbow fracture-dislocations, the initial treatment should be aimed at restoring normal bony architecture of the joint. In closed injuries (such as elbow dislocation treated with closed reduction), a period of observation is considered. If there is no clinical recovery by 8 weeks, exploration of the nerve is recommended. In more severe trauma or when open surgery on the proximal radius is contemplated, formal exposure of the PIN is recommended.
-
In atraumatic cases,
-
Nonoperative
- Activity modification
- Rest
- Painkillers
- Splinting for the hand
-
Operative
- Surgical decompression (neurolysis) is recommended if there is no clinical recovery by 8 weeks and more expediently if
- there is progressive weakness
- there is a space-occupying lesion
- For delayed presentation, tendon transfer is a reconstructive option to restore fingers and thumb extension.