What is neuralgic amyotrophy?
It is also known as
- Parsonage-Turner syndrome
- Paralytic brachial neuritis
- The shoulder-girdle syndrome
- Serratus-magnus palsy
- Acute brachial radiculitis
What causes it?
The actual cause remains unknown. It is believed to be mediated by an autoimmune process (the immune system of your own body attacking the nerve - which is similar to having a rebel army now attacking its own country!) but this is difficult to prove. The nerve is believed to be inflammed hence the term "neuritis". There are a number of risk factors which could precipitate the onset:
- Infection
- Trauma
- Surgery
- Acute illness
- Immunisation
The best description of the condition was provided by Parsonage & Turner in 1948 ...
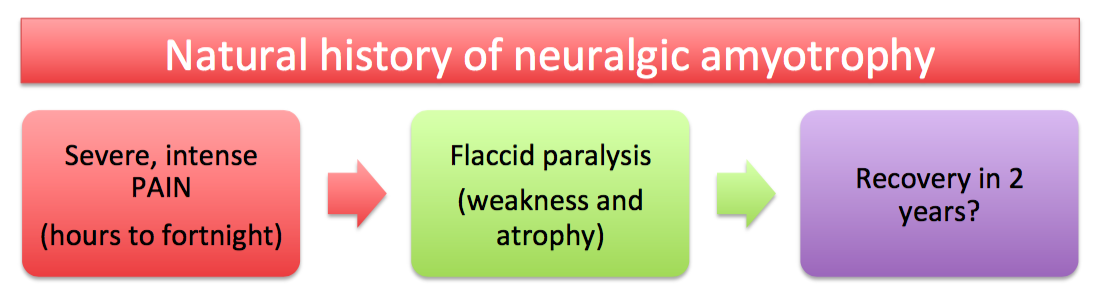
"without any constitutional disturbance pain starts suddenly across the top of the shoulder-blade and may radiate down the outer side of the upper arm or into the neck. This pain lasts from a few hours to a fortnight or more, and then a flaccid paralysis of some of the muscles of the shoulder girdle and often of the arm develops, and in some cases there is a patch of numbness over the outer side of the upper arm. When the paralysis appears, the severe pain usually stops, but a dull ache may persist considerably longer."
Classic description by Parsonage & Turner, published in Lancet 1948.
The involvement could be:
- Single peripheral nerve - commonest nerve involved is long thoracic nerve
- Multiple peripheral nerves - commonest combination is suprascapular and axillary nerves
- Nerve roots - common roots are C5, C6
- Spinal cord
- Bilateral
Investigations
- Neurophysiology
- EMG showing evidence of muscle denervation (fibrillations, positive sharp waves).
- NCS showing patchy sensory disturbance in the limb.
- MRI - can show oedema changes in denervated muscles
- Rarely in cases with positive family history or those with recurrent episodes, genetic testing may be requested.
Treatment
Nonoperative
- Painkillers (initial stage)
- Physiotherapy
- Observe for spontaneous resolution and recovery
Operative
- Recovery of muscle function and strength may take up to two years or possibly longer.
- Surgery (neurolysis +/- nerve transfer) could potentially shorten the period of disability and may be considered if:
- there is persistent impairment of function due to the muscle weakness.
- progress has plateaued with physiotherapy.